Epilepsy in Hiding
Did you know you can have epilepsy for decades and not know it? Turns out that’s true. I am Exhibit A.
It started with a twitch. I have a neck twitch. Weirdly, my twitches are unrelated to my epilepsy and they have now been diagnosed as something else–despite that being the family joke for years. But the twitches put me on the path to the epilepsy diagnosis. And in true ✨️Megan Fashion✨️ I did it backwards from most patients. Sigh. Haha.
I’ve been in a specialized type of physical therapy (PT) for my dizziness (at least that’s what it started for), and extreme fatigue, and I’ve found out there are other issues through this PT. It’s been so incredibly helpful.
I LOVE my physical therapist. She is one of the most helpful and open-minded providers I’ve ever had. She’s listened (and listened and listened, lol) to my various complaints and has helped me find the right avenues to figure out what is wrong whenever something new pops up. And I like to think we’ve bonded over our neurodivergent brains. hahaha
This story is a prime example. 🙂
I Get Twitchy Sometimes

In an appointment in the Spring of 2023, I mentioned that one of my exercises was particularly triggering to my twitch and my PT doctor was confused. “What twitch?” she asked. I was confused. How did she not know about my twitch? I’d been coming for almost two years. How had she not noticed it? I twitch many times a day. And I ask most doctors about it…or at least mention it to them. So she asked about my twitch at that appointment.
No, I don’t lose consciousness. It’s usually in my neck, but sometimes in my face and/or arms, or legs. Usually on the left, but occasionally on the right. The twitches happen more often when I’m tired. And talking about it makes it worse. Just talking about it made it happen a bunch in that few minutes. I get quite embarrassed when it happens a bunch of times in a row and I know someone sees it. It’s usually a quick motion of my head, so it’s not always seen, but sometimes it’s repeated several times in a row, which can be annoying. Fortunately, it doesn’t hurt.
My PT asked if anyone had ever identified it, or if I’d seen anyone about it. Yes, I’ve asked multiple doctors (I’ve lost count, I usually mention it when I think it might be relevant) and no, no one has ever had an answer. She asked a few more clarifying questions and smiled slowly.
My Twitch has a First Name…
“I think I know what it is.” She went on to describe the condition, which mirrored my experience. She said it’s essentially a software issue with my brain, rather than a hardware issue (like a brain tumor or MS would be). It’s a legitimate neurological condition. I’m not crazy. And it’s real. But what was the name?! I was dying to know there was a name for what it was. She finally said, “Functional Neurological Disorder.” (FND)
Well, that’s the lamest and most unidentifying name ever,” I laughed. But I also felt the cool relief run through me that there was a legitimate name for what the twitch was.
A Series of Fortunate Doctor Appointments
My PT suggested that I see a specific neurologist at my hospital, who is an expert in the condition and could be the one to diagnose me. Perfect! I sent a message to my Primary Care doctor (she’s also wonderful) and asked her to make the referral.
A few weeks later, I had the ovarian cyst issue. Fortunately, I had a follow-up appointment with my Primary Care doctor a week later that July, so I reminded her about the referral request, which she sent in during my appointment. When I followed up with the Movement Disorder clinic where this doctor is, they said it would be nine months if I was lucky. Sigh. But then a few months later, I was lucky enough to get a cancellation and my appointment was scheduled for November.
I included all this about the timing to just show how long it is to be in limbo. How long it takes to go from appointment to appointment. It’s mentally exhausting, for sure. And I have it easy. I have excellent insurance that is generally willing to approve visits and tests, and (if I pay for the premium plan) a wider range of doctors on my insurance’s authorized list. I’m jumping ahead a little, but it’ll be just over a full year from that first conversation about my twitch with my PT to when I’ll get the week-long EEG done for epilepsy testing. A YEAR. What in the SAM HILL is happening here–that it takes a year to confirm epilepsy from the first conversation with a provider. Anyway, I digress. [clumsily climbs off soap box]
The FND Doctor Appointment
In November 2023, I met with this new neurologist, who was as great as my PT said she would be. 🙂 She confirmed the FND diagnosis, so that was nice to finally have an answer for my twitches.
In questioning me about my twitches, she asked me if I ever had audio hallucinations. I said no. But I thought of times when I had smelled things that hadn’t actually existed. So I told her about that. “Olfactory Hallucinations” turns out are a thing. So that’s fun. Guess I’ve been having them since probably high school? Maybe longer? I smell raw chicken, or raw pumpkin (both smells I hate and make me nauseous), or smoke–like electrical smoke or wood smoke. None of the smells happen at the same time. She asked me about the last time this happened.
The last time this had happened had been about 6-8 weeks before. My roommate and I were both home and I thought I smelled electrical smoke. I felt very anxious and compelled to find the source. I wandered around the house smelling for it but found nothing. My roommate and I both checked around the house and neither of us could find anything. I kept smelling it, but couldn’t source it. My roommate smelled nothing at all. It was stressful for me! What if there was a fire in the walls and we couldn’t find it!! Deep breaths. I remembered the whole thing, still do, and there was no blacking out.
These instances don’t happen very often. But I remembered this was not the first time I’ve thought I smelled smoke in my house when nothing was burning and been super anxious there was a fire in the walls–and there wasn’t. It’s happened multiple times in my life.
Another Referral
After I explained this instance, the doctor said she wanted to refer me to the seizure clinic just to make sure I was not having seizures. She said it’s possible that these instances are part of migraines, but they might also be seizures, so we need to make sure they weren’t. She made the referrals to the Seizure Clinic, a brain MRI, and an EEG to test for seizures.
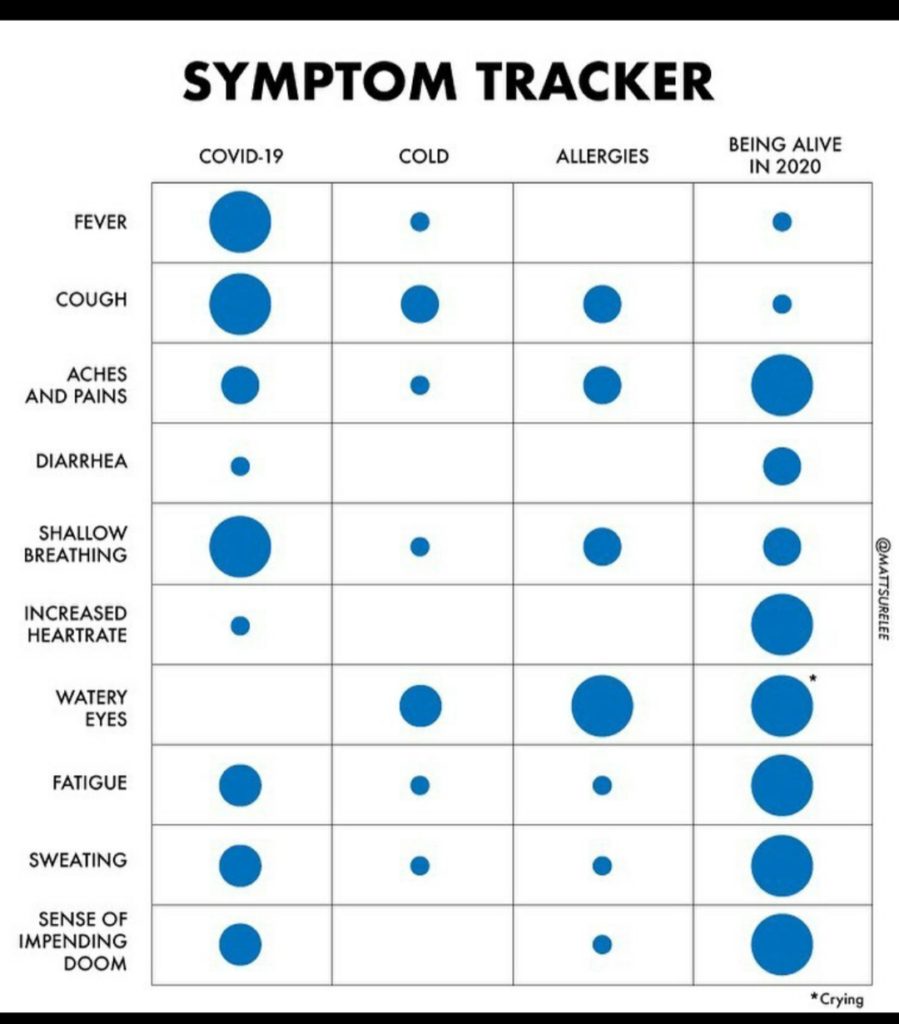
I was flabbergasted. Was it possible I was having a seizure and didn’t know it? Was that a thing in epilepsy? I knew of only two kinds of epilepsy: petit mal and grand mal seizures. And I wasn’t losing time, so I didn’t think I was having those. I wrote it off as an overly cautious doctor and agreed to go. BUT I would rather have an overly cautious doctor who ordered tests and made referrals than a doctor who ignored things I was concerned about. I’ve been wrong about so many things about my body that turned out to be symptoms. Clearly, I don’t know anything about my body. Haha!
More Testing
In January 2024, I had the MRI (which was a whole thing), and the EEG. The neurologist messaged me after both and noted that they both came back clear with no abnormalities noted. Wonderful! I wasn’t having seizures! Or at least the tests didn’t catch any… I felt confident that the one thing I didn’t have to worry about now was seizures. We can move on. Yay!
I came so close to canceling my appointment with the Chief of the Seizure Clinic. I was absolutely convinced he was going to say I’m not having seizures. Why put myself through another appointment where another doctor was going to shrug their shoulders, at best, and say, “That’s weird, not sure why that’s happening,” and send me on my way. At worst, I’d get the “you’re wasting my time” brush off almost immediately and the doctor wouldn’t even spend any time on me if they didn’t believe me, or try to gaslight me into convincing me I’m wrong. I’ve seen all of these kinds of doctors through the years. Sigh. My chronic illness patient friends will know all about these kinds of doctors. They know doctors like my PT doctor, my primary doctor, and my FND neurologist are rare unicorns. 💜
The Seizure Clinic Appointment
So I walked into the appointment fully, 100% expecting to hear, “Congrats! No epilepsy! and Goodbye!” Instead what happened was interesting and better, and kinda worse.
The doctor did a full neuro workup (awesome!), asked me my history, and asked me about the symptoms that had me referred there. I was very grateful he took this seriously despite my clear tests. I wasn’t getting the brush off! With a bit of relief, I went through them again. I remembered, that I occasionally had auditory hallucinations–where I’ll hear music I almost recognize or remember, or can sing/hum the lyrics but can’t quite remember. I let him know about that too.
After we went through all this, the doctor sat back, “Well, I do think you’re having seizures.”
I’m sorry, “WHAT?!”
I’m not sure I’ve ever had a more clear jaw-dropping moment in my life than that one to this point. Like comically so. It would have been hilarious to watch from the outside.
“Yes, your symptoms are consistent with epilepsy.”
I was reeling. “But my tests were clear…”
“That happens sometimes. That just means you didn’t have a seizure while the tests were happening.”
“I’m sorry, can you clarify? Are you diagnosing me with epilepsy?”
“Yes.”
I blinked and blinked and blinked. What was I supposed to do with this information? I still don’t really know what to do with this diagnosis, even now weeks later.

The Plan Moving Forward
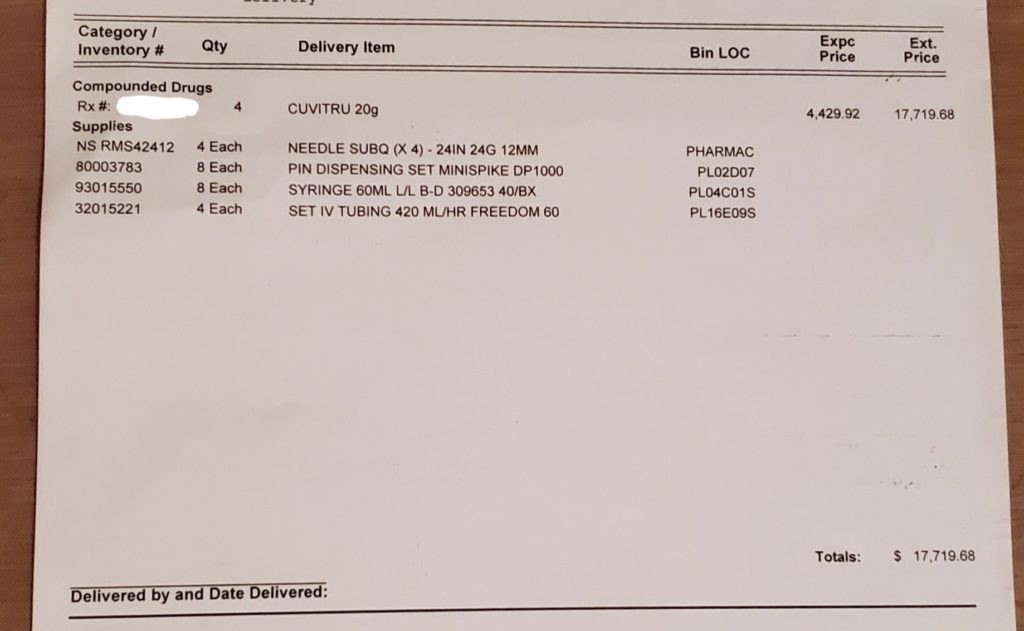
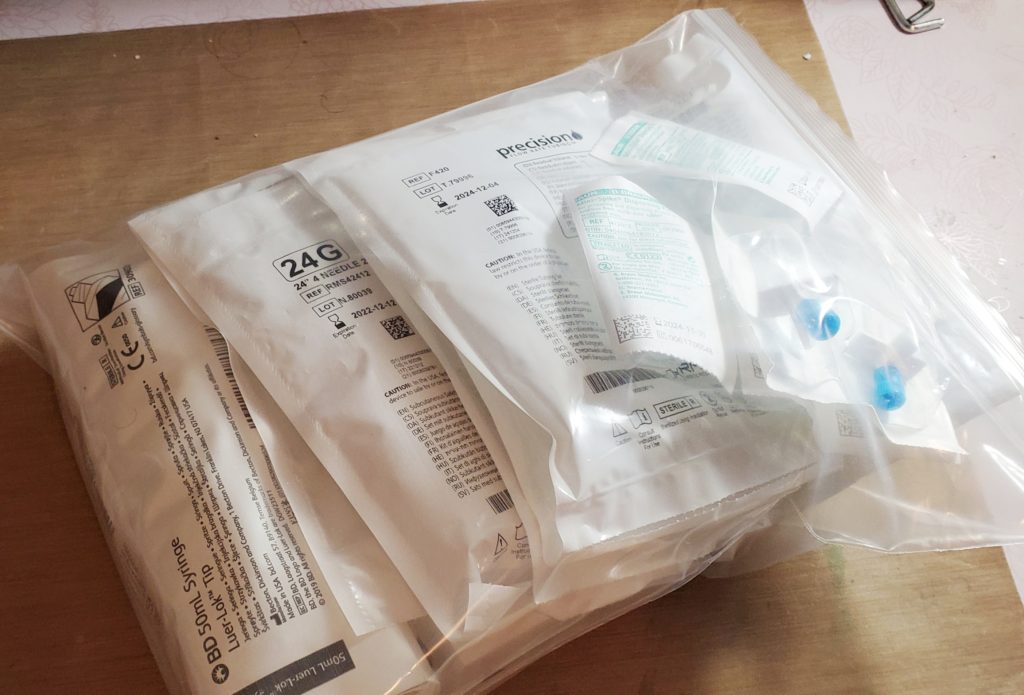
Part of the reason my headaches have been getting worse over the years was because of the seizures (very helpful to know, lol!). He said that one of my meds is also conveniently an anti-seizure medication, so he upped my dose. He said that the reason I’ve had fewer seizures in the past few years is likely because I started the medication and we had been slowly increasing the dose.
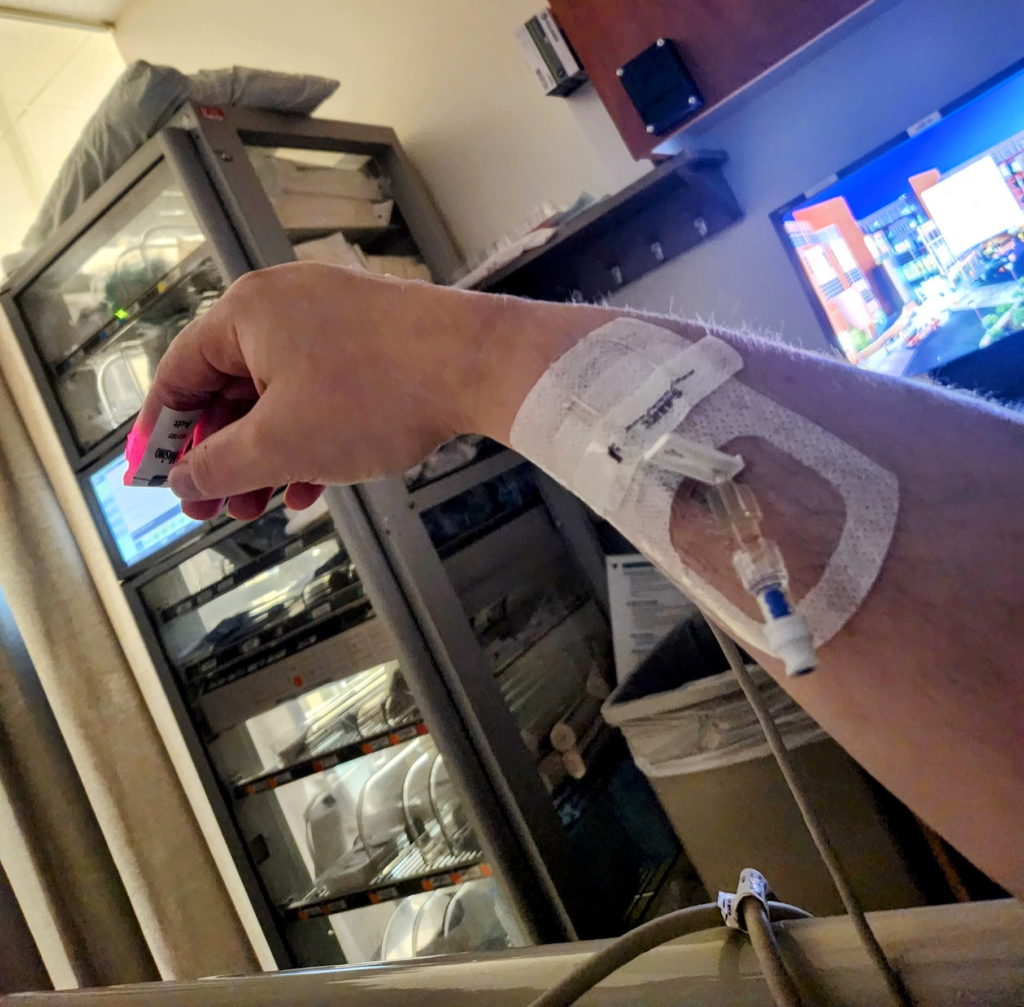
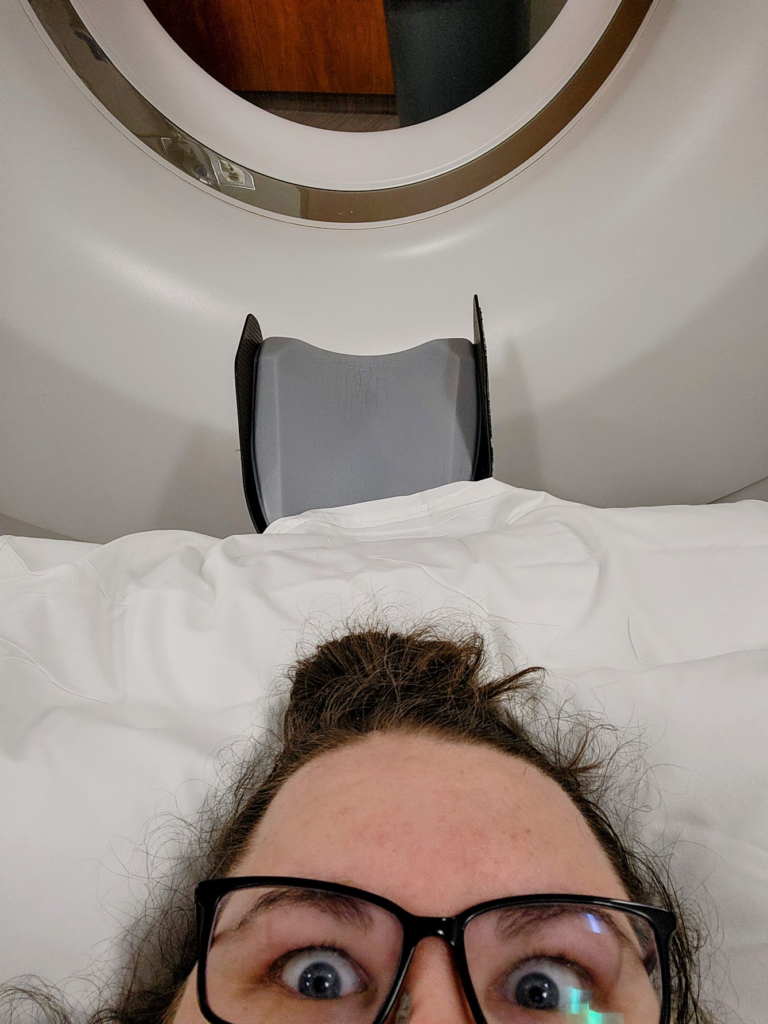
The doctor also said that he wants me monitored for a week in the hospital on an EEG to confirm the epilepsy diagnosis. A week in the hospital! I could still work from the hospital, so that’s good. It would be another 3-4 months out. sigh. (Spoiler–it ended up being a 5-month wait–and over my birthday, so that’ll be…fun. lol) I’m not looking forward to this and I’ll be bored. But as my mom said, I’ll get to stay at a 5-star “hotel” with all my meals catered and room service for my birthday! I’ll be waited on by my own personal wait staff (love you nurses and CNAs!!). And I like the hospital’s creme brûlée, so it’ll work out. 🙂
Still shocked, I couldn’t think of any questions except: could I keep my license? I had been worried about this. Fortunately, the doctor said I could, since I don’t lose consciousness. WHEW. Such a relief.
I was sure there was a ton of information I needed, but it was subtly clear the doctor was anxious to get out of there, so I didn’t ask any more questions. After the nurse came in and handed me my check-out paperwork (“Don’t call us, we’ll call you to schedule a follow-up”, uh, okay?) I realized I didn’t even know what kind of seizures I was having. I was so overwhelmed and confused.
What Now?
It would have been nice if the doctor or nurse had provided me with resources or even pointed me in the direction to get more information. Fortunately, I’ve been diagnosed with enough conditions that I know how to do medical research and how to find reliable resources. But in that moment, it would have been nice to have something in my hand and someone knowledgeable to talk to. Anyway. So I did the next best thing: I called my resident on-call nurse.
I called my mom. I think she was more shocked than I was. Can’t imagine why. How do you miss that your kid is having seizures?? lol. To be fair, I never told her about the very weird olfactory and auditory hallucinations. When I was a kid I wasn’t quite sure they actually were happening so I usually just brushed it off, in my defense. They were short and did not happen together or super often. I just always thought they were a weird “Megan Quirk”™ and I had so many “quirks” (which were, surprise, symptoms of all my different conditions) so why bring up another one for a doctor to shrug or roll their eyes at.
Turns out that hallucinations were one that I should have mentioned. OH WELL. hahahaha. And in researching epilepsy since then, I’ve had some other symptoms since childhood too, like a lot of deja-vus, near-constant and worsening headaches, and apparently seizures that have auras with my other senses.
Congratulations on Making it to the End
I found out from my doctor’s chart note that I have focal aware and focal absence seizures (probably because they are probably happening in my sleep too–sometimes a smell or a loud noise has woken me up). These are the most common types of epilepsy–I’ve learned this from researching epilepsy on my own.
So remember days ago at the beginning of this post when I said that I go about things backwards? Usually, people go in for seizures and walk out with an FND diagnosis. Well, I walked in for an FND diagnosis and walked out with an FND AND an epilepsy diagnosis. #onbrand
There you have it. I have epilepsy. Fortunately, it seems fairly well controlled (I think??) and doesn’t seem to really impact me much. If you see me panicking over the smell of raw pumpkin and it’s March–just tell me to chill out and it’ll pass in a minute or two. It’s just a little seizure. 😀
If it’s October–well that’s just (probably) because I hate the smell!
Disclaimer: I’m not a doctor and this is not a way to be diagnosed. 🙂 If you think you are having symptoms that sound similar, please find a doctor who will listen to you and take you seriously. You are your own best advocate. 💜