Today (Leap Day!) is Rare Disease Day so I thought I’d share my experiences having a Primary Immunodeficiency and being on immunoglobulin therapy. Two years ago I started weekly immunoglobulin therapy. It’s been quite the journey.
Getting a Diagnosis
When I was diagnosed with MCAS in the Fall of 2015, one of the things my immunologist and I discussed was my frequency of chest colds. Blood work looking for immunodeficiencies was normal (of course they were, sigh). Over the next few years, I continued to get chest infections that would trigger mast cell reactions. After several rounds of immunoglobulin labs with normal results (ugh), my immunologist wanted to try another round of labs that involved getting vaccinated. The lab tested my levels of response before and six weeks after the pneumococcal vaccine. I had little response after. And I anaphylacted to the vaccine. Ah, so not only is my body “blind” to pneumococcal, but I’m allergic to it. Of course I am. So no more pneumococcal vaccines for me. But I definitely recommend and encourage other people to get vaccinated, if you can!
We *finally* found the answer! I have Specific Antibody Deficiency (“SAD”) and my body doesn’t see streptococcus/pneumococcal bacteria. Basically I get chest colds almost anytime anyone sneezes near me. Getting the diagnosis was like another piece of my medical puzzle clicked into place. And yes, my family has teased me plenty for having a SAD diagnosis on top of everything else. Hahaha
Some months before, my doctor and I were discussing alternative treatment ideas. I felt like I was not getting ahead of my MCAS reactions. I had been doing some research and had heard some people had good luck with IV immunoglobulin (IVIG) therapy, so I brought it up to my doctor. He hedged a bit and said that he wasn’t aware of any studies that showed IVIG as a treatment for MCAS. He didn’t think my insurance would cover it, since it wasn’t an FDA approved treatment, and he warned it was expensive.
Getting Started
With the new diagnosis of SAD, I was now eligible for immunoglobulin therapy to be covered by my insurance (not all insurances cover SAD). Whew.
Treatment for immunodeficiencies is immunoglobulin therapy–which is derived from human plasma–which is donated, like blood donations. Plasma is processed and filtered to get just the immunoglobulin. Then 10,000 or more donations are combined together in order to get adequate immunoglobulin coverage. IVIG is typically administered via an IV once a month. Basically this treatment is supplementing and boosting my own body’s immune response. It’s covering the gaps. You can learn more about it here. There has been a national shortage and some people haven’t been able to get their infusions (I’ve been lucky). Please donate, or encourage others to donate!
My doctor and I discussed IVIG options and he felt that monthly IVIG would be pushing my body too much and not protect my immune system enough before the next dose, so we decided weekly subcutaneous (SCIG) infusions would be best. They can be done at home and the immunoglobulin is injected with small needles under the skin. They generally are tolerated better and are easier to manage. Both of those sound good to me!

So we gave it a try. The drug company provided a 4-week trial while insurance approval was pending. I started the Cuvitru trial within a week of diagnosis. The company made arrangements for a delightful nurse to come and teach me how to do the infusions.
My insurance approved immunoglobulin therapy. Yay! But they wouldn’t approve Cuvitru because it wasn’t on the formulary. So I was going to have to switch to Hizentra–a comparable immunoglobulin with preservatives, something we were concerned I would react to. Ugh, but okay.
Then I tried to make arrangements for a nurse, the medication, and the supplies–all of which are necessary. (The nurse was necessary till I felt comfortable doing the infusions on my own. Now I only use them occasionally when I need to do them in my back.) Well, the only “approved” pharmacy that the insurance would approve to distribute the immunoglobulin wouldn’t provide the nurse or the supplies. What?! And the insurance wouldn’t approve me to use the infusion clinics that were on the in-network list?! WHAT?! At least 65 phone calls later (not exaggerating, I counted), I was finally able to get an exception approved to use an infusion clinic on the approved list. I hope you hear my eyes rolling through the computer. It was painful and so frustrating. BUT, it got taken care of in time that I didn’t miss a weekly dose. Whew.
When I got my first statement from the pharmacy I was shocked. It was just under $20,000. For ONE MONTH of 25 grams of Hizentra immunoglobulin and supplies. The supplies were only $200ish. Fortunately, with my insurance coverage and then the copay assistance coverage from the pharmaceutical company, I only pay a tiny portion of that.
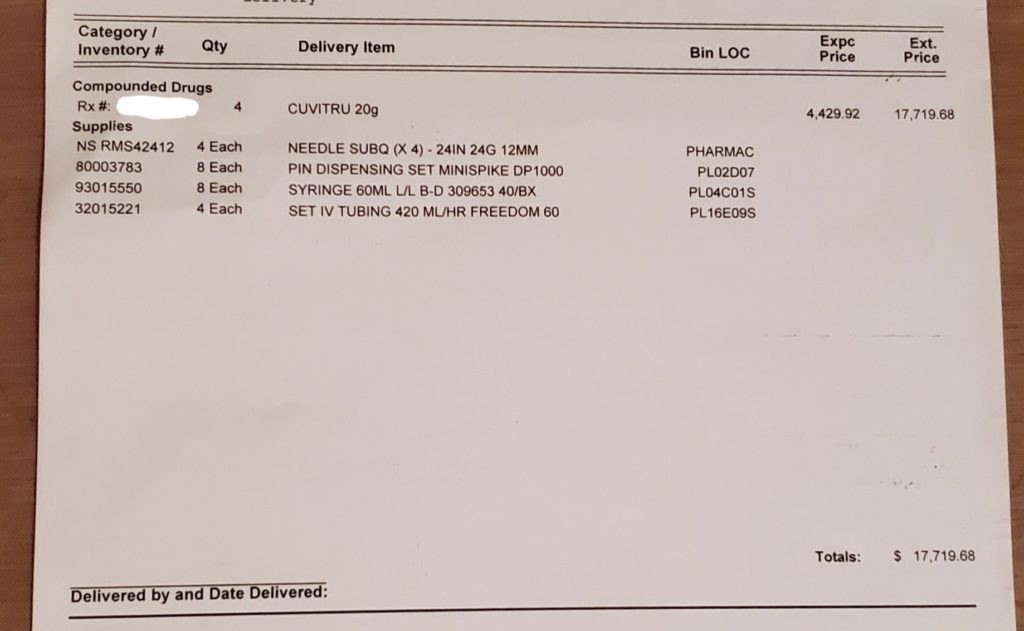
I just got my next summary statement from my pharmacy. They forgot to bill me for supplies, I think. But my medication is $4,430 a week. That’s $221.50 per gram. Just for perspective, the price of gold per gram (as of this post) is $51.07. Yeahhhh. There’s a reason immunoglobulin is nicknamed “liquid gold.”
Treatment

Right away I noticed I was not tolerating the Hizentra as well, but I wasn’t having severe reactions so I had to stick with it. Thank you benadryl (new band name; I call it!). Because I was doing infusions by myself, I could only do them in my abdomen or thighs. It became quickly apparent that my infusions are way slower than they should be according to some magical math equations. We still don’t know why what should be a 2-hour infusion takes almost 5 hours. So we tried adding more needle sites to try to speed it up. So at one point, I was doing 7 sites a week. My abdomen wasn’t having it. Every time I did it there, I would end up with horrible bruises, swelling, and itching that would last several weeks. I finally just stopped doing it in my abdomen. For over a year, I did infusions alternating between each thigh and changing the sites’ locations.

During all of this, my pharmacist was fantastic. He has worked so hard trying to find ways to make this work for me. Trying different needle lengths (switching between 9mm and 12mm) and flow rates. Trying varying numbers of needle sites and locations on my body. My immunologist over time also lowered my dose a few times to see if that would help too. But over time, the infusions in my legs became more and more painful to the point that my thighs constantly ached all the time.
I told my immunologist my concerns and he thought it might be time to switch medications to Cuvitru (the preferred medication). But remember how the year before it wasn’t on the formulary for my insurance? I reminded my doctor. “Formularies change. I think we should at least ask. Sometimes they’ll approve it if they know you aren’t tolerating the approved one.”
Lo and behold, they did approve it! And they covered it! (That was also a big concern.) So I switched and it’s been much better. I have also reduced the number of sites down to four and just deal with the infusion taking 5 hours every Saturday evening. These together have helped and my legs only sometimes hurt now. I think what has happened to my legs, especially my left, is that the weekly puncturing with so many needles has caused scar tissue to build up. If I pick the wrong spot, it can be really painful to try to insert the little needle.
Let me just tell you–there’s helpful introductory video that one of the drug companies created that shows how to do an infusion. But it also cheesily shows a man strolling down the street all casually walking his dog like it ain’t no thing to be pumping medicine into his abdomen. “You can do anything while you do infusions!” Ha! Yeah right. I feel yucky during and after these infusions. And generally do not feel up to strolling down the street. I have run some quick errands, but try not to do so. DoorDash is the best on Saturday nights. 🙂 And then I sleep for 10-14 hours after. It’s exhausting.

My pump, pump bag (underneath the pump), thermometer, and a little storage container full of odds and ends like alcohol wipes, cavilon wipes, bandages, gloves, extra supplies, etc. The drug company sent me a free laptop type bag to store everything in. Makes it easy to travel with too! And yes, I’ve flown with my medication and supplies–it wasn’t a problem! 
A month worth of medication to be stored in my fridge. 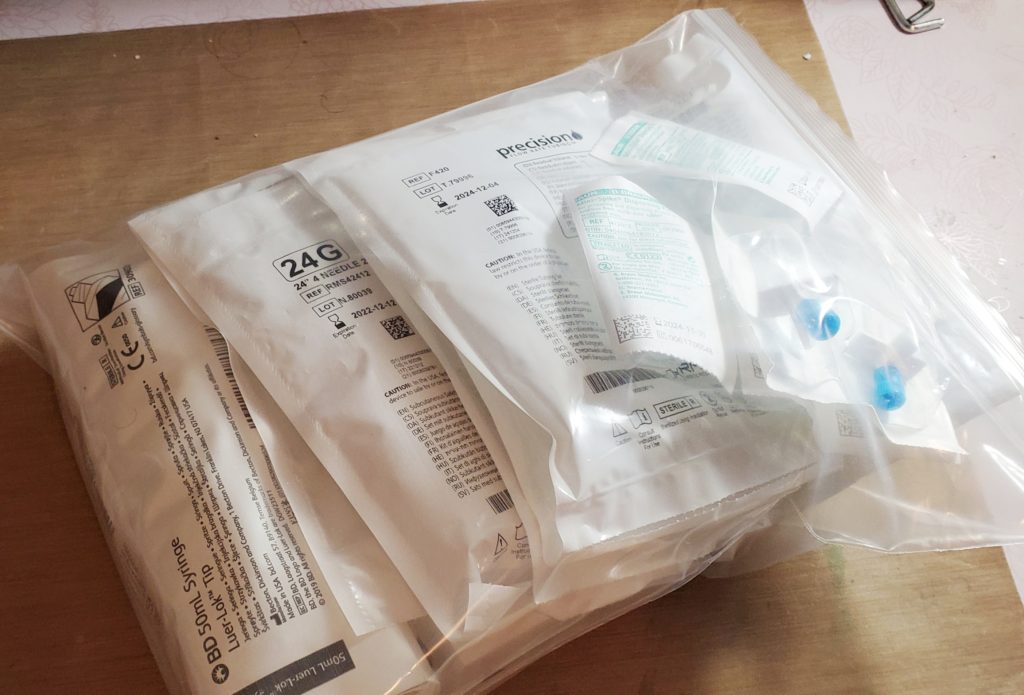
A month worth of supplies. I also have tons of extra supplies on hand because sometimes something is missing or I accidentally contaminate something. 
Kitting my supplies into weekly bags so each week I have everything I need for that infusion. Makes things a lot easier!
Two Years Later…
My current regimen is 20g of Cuvitru weekly. The goal has been to find the lowest level of immunoglobulin I need to stay healthy. With the severe cold I got this winter, I think we might have hit my lower threshold. Bummer. I was hoping to get to a lower dose (lower dose = lower cost). Oh well.
But overall, the immunoglobulin therapy has helped so much. I haven’t gotten sick nearly as much, or as severely. Getting sick was a big trigger for me on several levels–so eliminating that has kept me out of the hospital and anaphylaxis free for 18 months. A new record! As hard as this treatment can be, it’s been worth it.
Unfortunately, right now there is no alternative way to treat primary immunodeficiency–which is why additional awareness or additional research is needed. You can support patients like me by donating plasma (sometimes you can get paid for it!) or donating to organizations like the Immune Deficiency Foundation.














